More states are using Medicaid to develop food-as-medicine initiatives, part of the strategy released by the Biden administration’s White House Conference on Hunger.

More states are using Medicaid to develop food-as-medicine initiatives, part of the strategy released by the Biden administration’s White House Conference on Hunger.
December 15, 2022

At the clinics run by Community Care Cooperative in Massachusetts, doctors and nurses can make a special kind of referral not often found in healthcare: When patients are struggling to manage an illness like diabetes because they lack the resources to prepare healthy meals, medical professionals can refer them to Project Bread, a local food-assistance organization. Then, one of 12 coordinators at the nonprofit will call the patient.
“We try to understand the range of barriers that are making it difficult for them to purchase, prepare, or store different, healthy foods,” explained Jennifer Obadia, Project Bread’s senior director of health care partnerships. Once the coordinators get a picture of an individual’s situation, they can send grocery store gift-cards and kitchen supplies or sign the patient up for cooking classes or nutrition counseling. They can even refer them to a service that will deliver “medically tailored meals.” Every three months, they check in on the patient.
In its first two years, the program served 5,000 patients, and a recent evaluation found that 25 percent were no longer food insecure after participating for six months.
Massachusetts was able to use a Medicaid waiver approved by the federal government to implement and pay for the program. Over the past few years, it was one of the only states using Medicaid—the federal healthcare plan for low-income Americans—to develop food-as-medicine initiatives.
That’s about to change. In addition to approving a continuation and expansion of Massachusetts’ program, this fall, the federal Centers for Medicare and Medicaid Services (CMS) approved similar projects in Oregon and Arkansas, and more state-wide projects are still to come.
The movement is a direct result of the recent White House Conference on Hunger, Health, and Nutrition, during which the Biden administration released a National Strategy to end hunger and increase healthy eating. Within the goal of “integrat[ing] nutrition and health,” the administration identified expanding Medicaid participants’ access to food-as-medicine interventions as a key approach. And while some components require Congressional action to move forward and will likely take many years to roll out, CMS is moving with surprising speed to approve state Medicaid waivers that make progress toward that goal.
“I think we’re on the precipice of some real systemic change when it comes to the healthcare system. It just makes sense to be making the connection between food and healthcare.”
And it’s not just CMS that’s moving relatively quickly: In October, the U.S. Department of Agriculture (USDA) held its first Nutrition Security and Healthcare Summit. A month later, the agency announced a $59 million investment that includes funding for produce prescriptions, where physicians can offer patients coupons for free fruits and vegetables to boost nutrients in their diet. Also in November, as part of partnership agreements made at the conference, Share Our Strength’s No Kid Hungry campaign and the American Academy of Pediatrics announced a project to improve how, and how often, pediatricians screen for food insecurity.
Additionally, this week, Senators Cory Booker (D-New Jersey) and Mike Braun (R-Indiana) held an Agriculture Committee hearing on food-as-medicine efforts and opportunities. During the hearing, Senator Roger Marshall (R-Kansas) said he is working on legislation that would expand food-as-medicine pilot programs in both Medicare and Medicaid.
State Medicaid projects are one piece of that bigger picture, and experts say that not only could they have a real impact on hunger and diet-related diseases in vulnerable populations, but they’re also a larger sign that the shift toward food-as-medicine may finally be accelerating.
“I think we’re on the precipice of some real systemic change when it comes to the healthcare system,” Obadia said. “The connections between food insecurity and poor nutrition and really costly and life-altering diseases like diabetes are so clear. It just makes sense to be making the connection between food and healthcare.”
For at least the past decade, a number of organizations have been pushing that connection. And over that time, the body of research that supports food-as-medicine interventions has been growing, said Katie Garfield, the director of whole person care at Harvard Law School’s Center for Health Law and Policy Innovation. “We’re actually expecting a number of larger studies to come out in the coming years,” she said.
Garfield pointed to a recent Food is Medicine Research Action Plan produced by experts from the Center and from the Aspen Institute. (Some institutions use the term food-is-medicine instead of food-as-medicine; they refer to the same efforts.) They summarized the research on three interventions: medically tailored meals, produce prescriptions, and medically tailored groceries—groceries designed to meet specific healthcare needs. Then, they identified key gaps.
Research on medically tailored meals is the most developed so far, they found, but all three interventions “are associated with reduced food insecurity, improved dietary intake, and improved participant mental health.”
In addition to more research on how critical food is to health outcomes, there has also been more attention to how healthcare outcomes are often worse for low-income families, many of whom are people of color. “The overarching goal of our waiver was to eliminate health disparities,” explained Lori Coyner, the senior Medicaid policy advisor for Oregon Health Authority (OHA), which administers Medicaid in Oregon.
And while there is a cost associated with running the programs, Coyner said she hopes that eventually they will lead to overall savings. “Our goal is that by providing things like housing and nutrition supports, we keep people out of the emergency department and the hospital,” she said.
So far, the research supports that approach. On medically tailored meals, at least, Garfield said there’s strong evidence on the benefits of investing in programs. One 2019 study she pointed to found that over the course of about a year, the meals resulted in 49 percent fewer inpatient admissions and a 16 percent cut in healthcare costs compared to a control group of patients who did not receive the meals. (During the Agriculture Committee hearing on Tuesday, Senator Marshall moved to enter that study into the record.)
In another paper published this fall, researchers used modeling to estimate that if all patients in the U.S. with mobility challenges and diet-related diseases received the meals, 1.6 million hospitalizations would be avoided, with a net savings of $13.6 billion annually.
There are many ways to fund food-as-medicine interventions. Massachusetts, Oregon, and other states including North Carolina and Arkansas are using a specific mechanism in Medicaid called an 1115 waiver, a tool that has long been available to states. These 1115 waivers allow states to use federal funds to test programs that wouldn’t normally be included under Medicaid.
At the nonprofit healthcare research group KFF (the Kaiser Family Foundation), Madeline Guth tracks those waivers, and she’s mapped 23 states that currently have approved or pending ones. She says states are increasingly using the waivers to fund programs that address what are called “health-related social needs” or “social determinants of health.” It’s a category that includes a wide range of non-clinical factors, including safe housing, water pollution, and access to healthy, nutritious food.
“It’s not brand new,” Guth said, “but the Biden administration has identified social determinants of health as being a top priority for the Medicaid program.”
The catch is that these programs are only available to a limited number of Medicaid participants. “We don’t have the funding to provide housing and food for everyone. There needs to be some sort of medical need.”
To that end, more states are helping patients with other health-related social needs in their pilot programs, including stable housing, while adding new food and nutrition support. While OHA has had an 1115 waiver in place since 1994, it did not include a specific food program. Clinics serving Medicaid patients could provide help in other ways, but the assistance was piecemeal.
“We learned that in order to have these services utilized in a more robust way, we needed to standardize them and make them part of the benefits for our members,” she said. OHA will be integrating food-as-medicine into its program through 2023, and similar to Massachusetts’ model, Coyner said it will involve screening done at health centers and working with partner organizations to deliver nutrition counseling and education, medically tailored meals, fruit and vegetable prescriptions, and pantry stocking.
The catch is that these programs are only available to a limited number of Medicaid participants. In OHA’s case, that means people experiencing major life transitions or disruptions that impact their access to healthcare. For an adult, that might include loss of housing. For a child, it may be an entry into the foster care system. “We don’t have the funding to provide housing and food for everyone,” Coyner said. “There needs to be some sort of medical need.”
That distinction sets these Medicaid food and nutrition programs apart from large federal programs like SNAP and WIC, which reach a much broader swath of the population. But the programs often help connect patients to those resources as a longer-term option.
In Massachusetts, Obadia said Project Bread’s coordinators talk to patients about whether they’re using SNAP or WIC. If they’re not, coordinators can help them confirm eligibility. “They can even walk them through the application process to make sure they’ve got all their documentation,” she said. “We’re really making sure that they’re utilizing all the resources available to them.”
In Project Bread’s evaluation, the organization found that after six months in the program, SNAP participation among patients rose from 64 percent to 72 percent. Another surprising finding in the evaluation was that a major barrier—even for patients already receiving SNAP benefits—was having the right kitchen equipment to store food and prepare healthy meals. Eighty-two percent of patients surveyed requested basic supplies including pots and pans, plates and bowls, and cooking utensils. Nearly 10 percent didn’t have a refrigerator.
All of that data is available because the federal government requires states using 1115 waivers to conduct evaluations of their programs. In addition to giving states the flexibility to experiment, Garfield said evaluation is one of the waivers’ biggest strengths, since that information can then be used to build more effective programs going forward.
“The only downside [to using Medicaid 1115 waivers to provide food and nutrition support] is the fact that it’s state by state,” she said. “My one overarching concern is that . . . some states will have it and some states won’t. So, there’s a risk of deepening some health inequities across the country.”
Garfield hopes that as more states try out these programs, the case for permanently incorporating them into Medicaid benefits will build. North Carolina and Arkansas are also already using 1115 waivers for food and nutrition, and Guth’s KFF tracker points to eight additional pending waivers that address social determinants of health (although they may not all include food).
“My one overarching concern is that . . . some states will have it and some states won’t. So, there’s a risk of deepening some health inequities across the country.”
Finally, the White House’s National Strategy also directs CMS to issue guidance detailing how states can use section 1115 waivers to test the expansion of food-as-medicine interventions. That, experts said, will likely help more states to get on board, driving a push for national adoption.
“If a number of states showed that providing housing supports and nutrition supports results in positive health benefits for members,” Coyner said, there’s more of a chance the federal government would incorporate it into overall Medicaid benefits.
For now, in Massachusetts, Obadia is excited about the fact that updates to the state’s most recent waiver will allow patients who are eligible for medically tailored meals to start receiving 21 meals per week instead of 10. It might not be a radical change, but each improvement is meaningful.
“I think addressing . . . . housing and food is a really effective and clever way of addressing health disparities,” she said, “because, in some ways, it’s starting to level the playing field.”
September 4, 2024
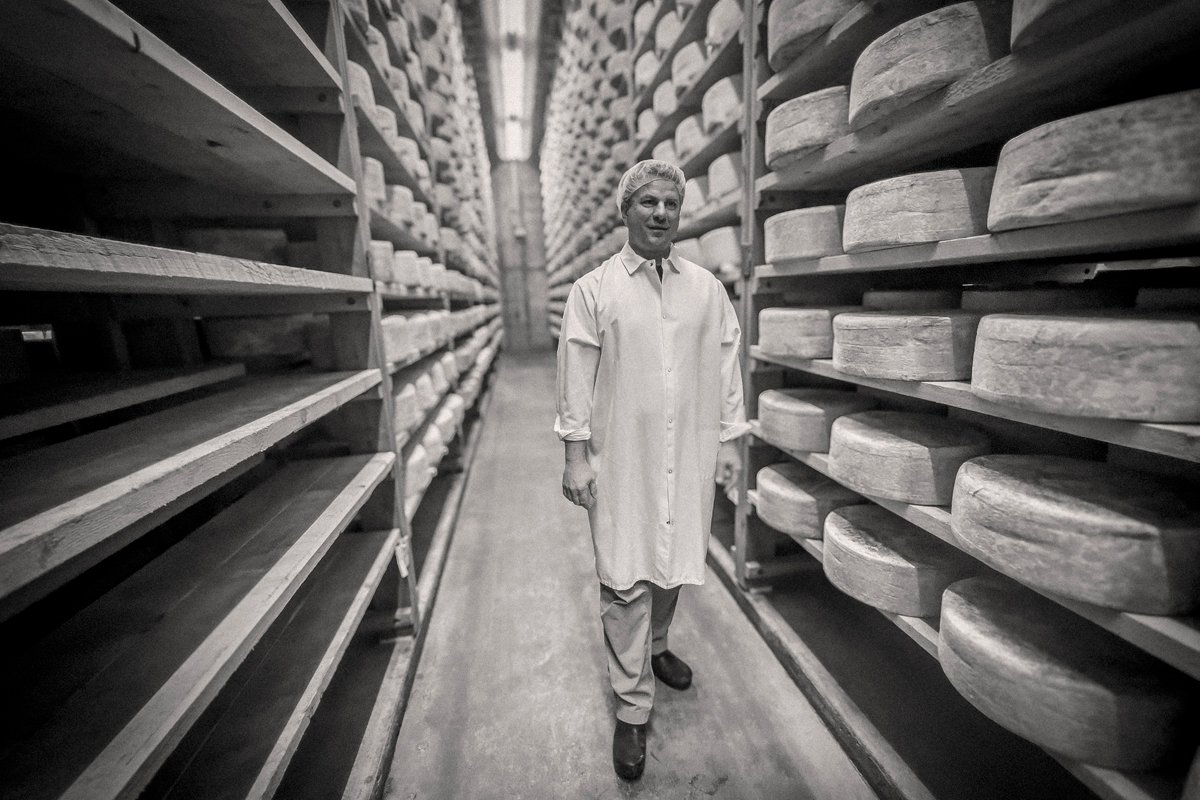
By paying top dollar for milk and sourcing within 15 miles of its creamery, Jasper Hill supports an entire community.
September 3, 2024

August 27, 2024

August 26, 2024

Like the story?
Join the conversation.