Eight months after advocates raised alarms about marketing materials for medically important antibiotics, nothing has changed to prevent uses that create resistance to life-saving drugs.

Eight months after advocates raised alarms about marketing materials for medically important antibiotics, nothing has changed to prevent uses that create resistance to life-saving drugs.
January 25, 2022

Antibiotic resistance—the development and spread of “superbugs” that can’t be treated with current medicines—is such a critical issue, public health experts say it represents “the next global pandemic.” They are also concerned that the current pandemic could undo some of the progress on the issue that the U.S. has already made. And since sales of medically important antibiotics to livestock producers are nearly double the sales of those used in human medicine, curbing overuse in agriculture is essential to reining in the rise of superbugs.
The U.S. Food and Drug Administration (FDA) is responsible for regulating the use of antibiotics in animals, and for years, advocacy organizations have called the agency out for moving too slowly to address overuse.
Now, they say the agency is allowing a drug company to openly flout rules intended to protect public health in its marketing material. And they argue it’s just one example of multiple loopholes that allow producers to feed antibiotics to animals for dangerous lengths of time.
“It looks like the FDA is unwilling to tell this company to stop marketing [their] drug to be used off-label.”
In May 2021, the Keep Antibiotics Working (KAW) Coalition sent a letter to the FDA outlining how Zoetis—a global company that makes medicines for livestock—encourages producers to feed Aureomycin to cattle in repeated five-day “pulses” to prevent Bovine Respiratory Disease (BRD), which likely violates FDA rules for the use of chlortetracycline, a medically important antibiotic that is the key ingredient in Zoetis’ product Aureomycin.
Eight months later, nothing has changed.
“It looks like the FDA is unwilling to tell this company to stop marketing [their] drug to be used off-label,” said Steven Roach, KAW’s senior analyst and the Safe and Healthy Food Program Director at Food Animal Concerns Trust (FACT). “They set that ‘do not use for more than five days’ for a purpose, and if the company can ignore that, it just undermines any efforts at FDA to control how these drugs are used.”
BRD is a condition that commonly affects cattle when they arrive at feedlots, when the animals are under stress and confinement accelerates the spread of pathogens. “Almost all of our cattle, we pulse with Aureomycin,” ruminant nutritionist Tom Peters says in a video on “starting cattle” posted on the company’s main webpage for feed additives. On another Zoetis website dedicated to BRD, the company promotes putting the drug in feed in five-day pulses and offers the example of a producer who always does two pulses, and if needed, “will do a third five-day pulse.”
FDA regulations only allow chlortetracycline to be fed to cattle for up to five days. Advocates say producers are getting around the limitation by pausing for a day or two and then starting a second “pulse,” but that this off-label protocol still violates the limitation’s intention.
“Less use is always better,” said Matt Wellington, the director of public health campaigns at the national advocacy group U.S. PIRG. And even if a producer is obtaining a new prescription to restart the feeding each time, “Pulse feeding sounds like just another way to get around appropriate antibiotic use,” he said.
Zoetis declined to comment for this article.
Over the past five years, the FDA has taken several steps to reduce the overuse of antibiotics important to human medicine in animal agriculture, including requiring veterinarian oversight of all medically important antibiotics given to animals, banning their use solely for the purpose of faster growth, and working toward setting duration limits for each drug. But the use of medically important antibiotics for disease prevention is still routine and widespread in beef and pork production, and this isn’t the first time a drug company has been accused of marketing agricultural practices that go against the agency’s regulations.
In 2015, the FDA sent a warning letter to a Zoetis competitor, Elanco, because its marketing materials encouraged pork producers to give healthy pigs a combination of two drugs to fatten them up, rather than to treat disease.
This time, Roach said the FDA met with KAW to discuss the group’s concerns but agency representatives would not discuss whether they planned to contact Zoetis. As of this writing, the company’s marketing materials haven’t changed.
When asked whether the FDA had taken any action related to the situation, a spokesperson merely said, “The FDA acknowledges Keep Antibiotics Working Coalition’s positions as articulated in its letter.” The spokesperson also shared the agency’s own guidance on the practice of “pulsing” antibiotics in feed, which essentially says the practice would qualify as “an illegal extra-label use” if a veterinarian authorized more than one five-day course off the bat. But if a farmer went back to the veterinarian after a five-day course of the drug and got a new authorization for a second course, it would be legal.
Zoetis’ marketing suggests to farmers that they should be thinking about additional “pulses” from the get-go, but it’s unclear how veterinarians are authorizing the process.
While farmers feeding their animals one drug for an extra five days may not be a huge issue on its own, the World Health Organization (WHO) identifies antibiotic resistance as “one of the biggest threats to global health” today. A 2019 Centers for Disease Control (CDC) report found antibiotic-resistant bacteria cause 2.8 million infections and 35,000 deaths annually in the U.S, and other estimates are much higher. A study published just this month found that in 2019, antimicrobial resistance played a part in 4.95 million deaths globally and directly caused 1.27 million of those deaths.
If we want to prevent those numbers from rising, the durations that antibiotics are administered for matter, said Sameer Patel, a pediatric infectious disease physician and Director of Antimicrobial Stewardship at the Ann & Robert H. Lurie Children’s Hospital of Chicago. “In human medicine, there is a huge push to essentially change our practice for a lot of conditions to use the shortest effective therapy to treat any infectious condition,” he said.
In the past, there was an accepted idea that antibiotics should be given for long periods of time to kill every bug and therefore eliminate the chance of a surviving bug developing resistance, he explained. And while that reasoning may still apply in certain cases, in the overwhelming majority of situations, physicians have learned that the shorter the duration, the better. This is because when antibiotics are given for longer, every organism in the body is exposed to the antibiotic, whether it’s the intended target or not, potentially creating “selective pressure,” which eliminates targeted bacteria but may give an advantage to non-targeted bacteria that already have resistance.
“It’s like evolution sped up,” Patel said. “They’ll be more likely to proliferate in the body and spread to other people. So the idea of the short duration is to remove that selective pressure as much as possible.”
The concept applies to both humans and livestock, since bacteria from animals can be passed to people through the air, water, and meat.
Chlortetracycline belongs to a class of antibiotics called tetracyclines that the WHO considers “highly important.” They’re commonly used in the treatment of Lyme disease in the U.S., and in other countries to treat respiratory infections, Patel said. While they’re not as critical as cephalosporins or penicillins, he explained, they are becoming more important in the treatment of infections caused by bacteria that have developed resistance to more common drugs.
“Essentially, they’re important back-up drugs for very resistant infections,” he said. “Having it as an option for those conditions when we need it is still very important.”
The FDA spokesperson said that “evaluating the potential for an antimicrobial drug to impact antimicrobial resistance in humans” is part of the process it undertakes to determine the appropriate amount of time each drug should be given to animals.
While the agency already determined Aureomycin should be fed to cattle for a maximum of five days, 30 percent of the medically important antibiotics currently used in agriculture have no “defined duration of use” or “duration limit.” In its current plan to combat the development of resistant bacteria, however, the agency has laid out a plan to set durations for the drugs that don’t currently have them.
For example, multiple versions of tylosin—a critically important antibiotic WHO categorizes as “highest priority” and which is sold by different companies—lack duration limits. Feedlot operators use it to prevent liver abscesses in cattle, and one study that evaluated antibiotic use on 22 feedlots between 2016 and 2017 found producers put tylosin in cattle feed for an average of 134 days at a time.
“We’ll keep having to play whack-a-mole . . . until the FDA addresses the root of it—overusing our life-saving medicines to prevent disease brought on by industrial farming conditions.”
Given numbers like that, public health advocates say the agency is moving way too slow. The FDA first announced it would work on “appropriately targeted durations” in 2016. In 2021, the agency published a “concept paper” that would be followed by “draft guidance.” According to its timeline, duration limits wouldn’t be completed until at least 2027. The agency said it would be “premature to speculate on a specific timeline for issuing the draft guidance,” noting officials are currently going through 38,000 comments.
“[Duration limits were] part of their five-year plan to address antibiotic resistance that they put out in 2018, and we still don’t have any significant progress to solve this problem,” Wellington said.
However, Roach at FACT says the Zoetis’ marketing of Aureomycin suggests that setting defined limits isn’t enough. The agency also has to have a system to enforce them, he adds.
In a response to a question about regulation, the FDA spokesperson deferred to “veterinary oversight” as adequate.
“We also need stronger regulation around veterinarians having to reevaluate any continued use,” Wellington said, which could address Aureomycin’s “pulse feeding” messaging.
And at the end of the day, Wellington sees Zoetis’ marketing as one of many small examples of how the federal regulatory system is only scratching the surface of regulating antibiotic use in animal agriculture rather than implementing larger systemic changes that would reduce the need for preventive antibiotics.
“Drug manufacturers and meat producers use semantics to bend [the rules around antibiotic use, and] the pulse feeding of chlortetracycline is another example of this,” he said. “We’ll keep having to play whack-a-mole . . . until the FDA addresses the root of it—overusing our life-saving medicines to prevent disease brought on by industrial farming conditions.”
September 4, 2024
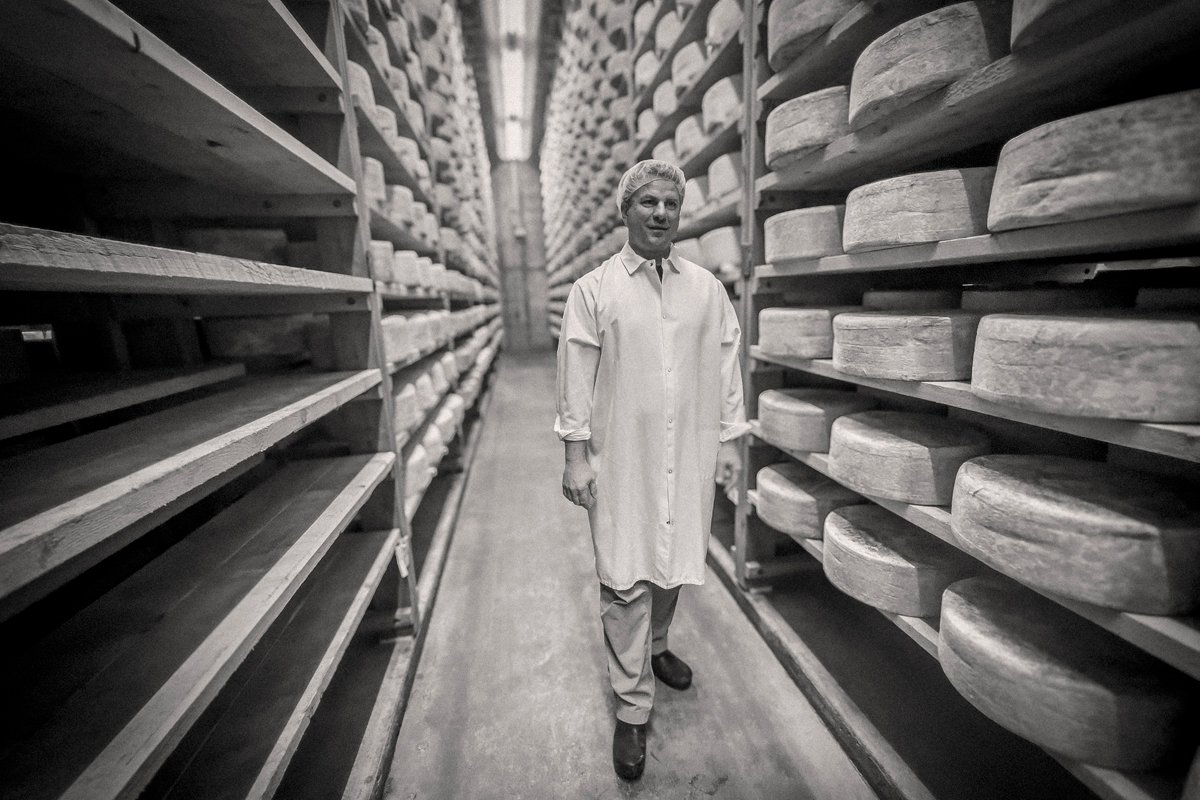
By paying top dollar for milk and sourcing within 15 miles of its creamery, Jasper Hill supports an entire community.
September 3, 2024

August 27, 2024

August 26, 2024

Like the story?
Join the conversation.